This project is still in progress
Thesis link
Thesis code repository
Problem description
Endovascular surgery is an alternative to open surgery, and it has fewer complications, such as:
- Shorter recovery time
- Benefit of local anesthesia instead of general
- Less pain and bleeding
Endovascular procedures typically rely on fluoroscopy for imaging, which uses X-rays, an ionizing radiation that increases cancer risk. Fluoroscopy also has limited soft-tissue visualization; for example, it cannot visualize blood vessels, the brain, organs, or muscles.
Magnetic Resonance Imaging (MRI) offers an alternative to fluoroscopy, providing excellent soft-tissue visualization without radiation exposure.
However, MRI is not widely used for endovascular procedures because:
- The images have low resolution and slow update frequency
- the endovascular procedure devices (guidewire, catheter) are not visible very well, raising concerns about the procedure's safety.
This project aims to improve the shortcomings of MRI-guided endovascular procedures. The following research question was raised:
How to improve the safety of MRI-guided endovascular procedures?
The research question was approached with the following objectives:
- Optimization of an Interactive MRI sequence for endovascular procedures.
- Detect MR-safe passive guidewire in real-time during interactive MRI sequence.
- Implement haptic feedback on the CathBot robotic platform.
Background
Endovascular procedures
CathBot
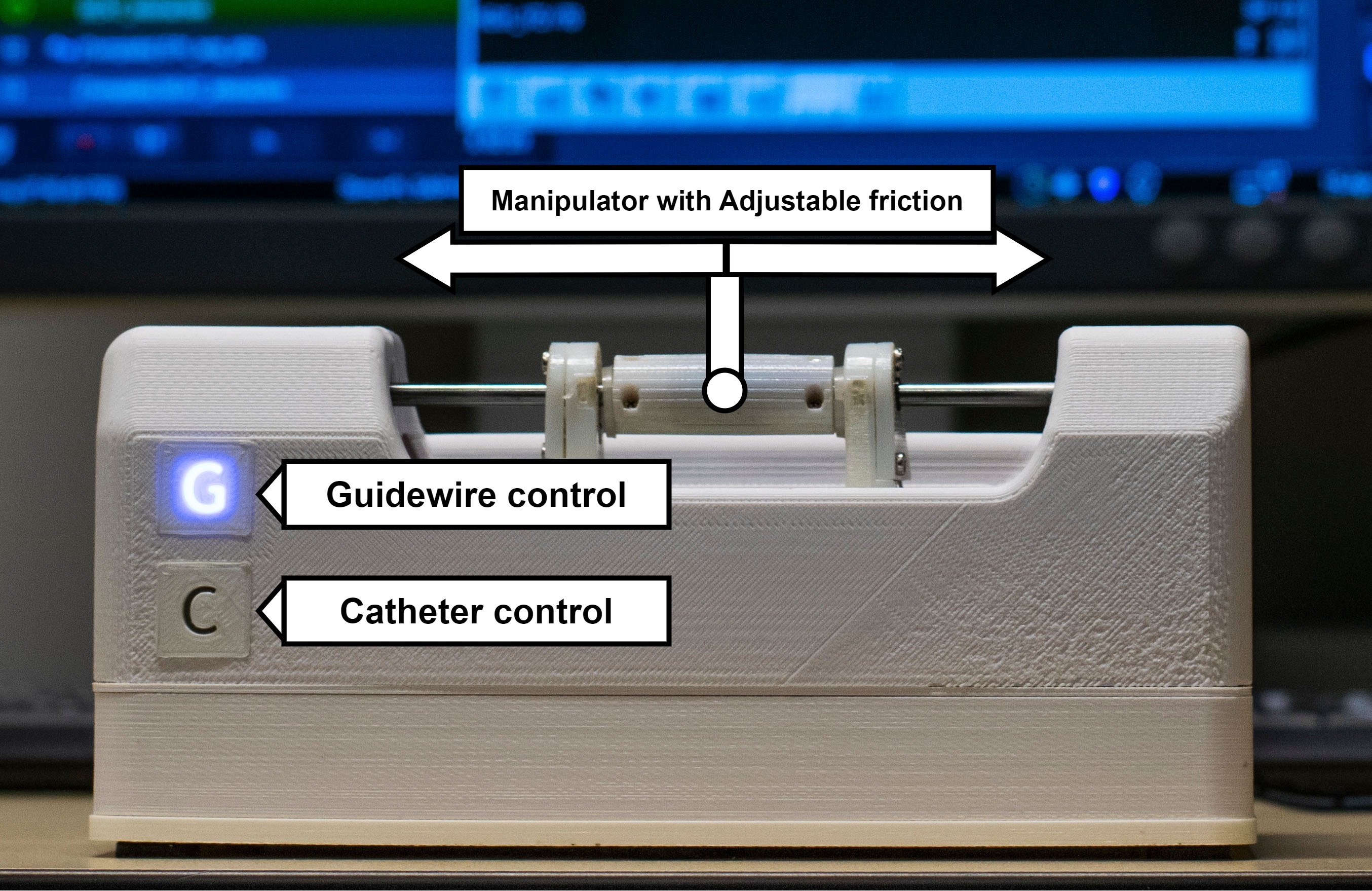
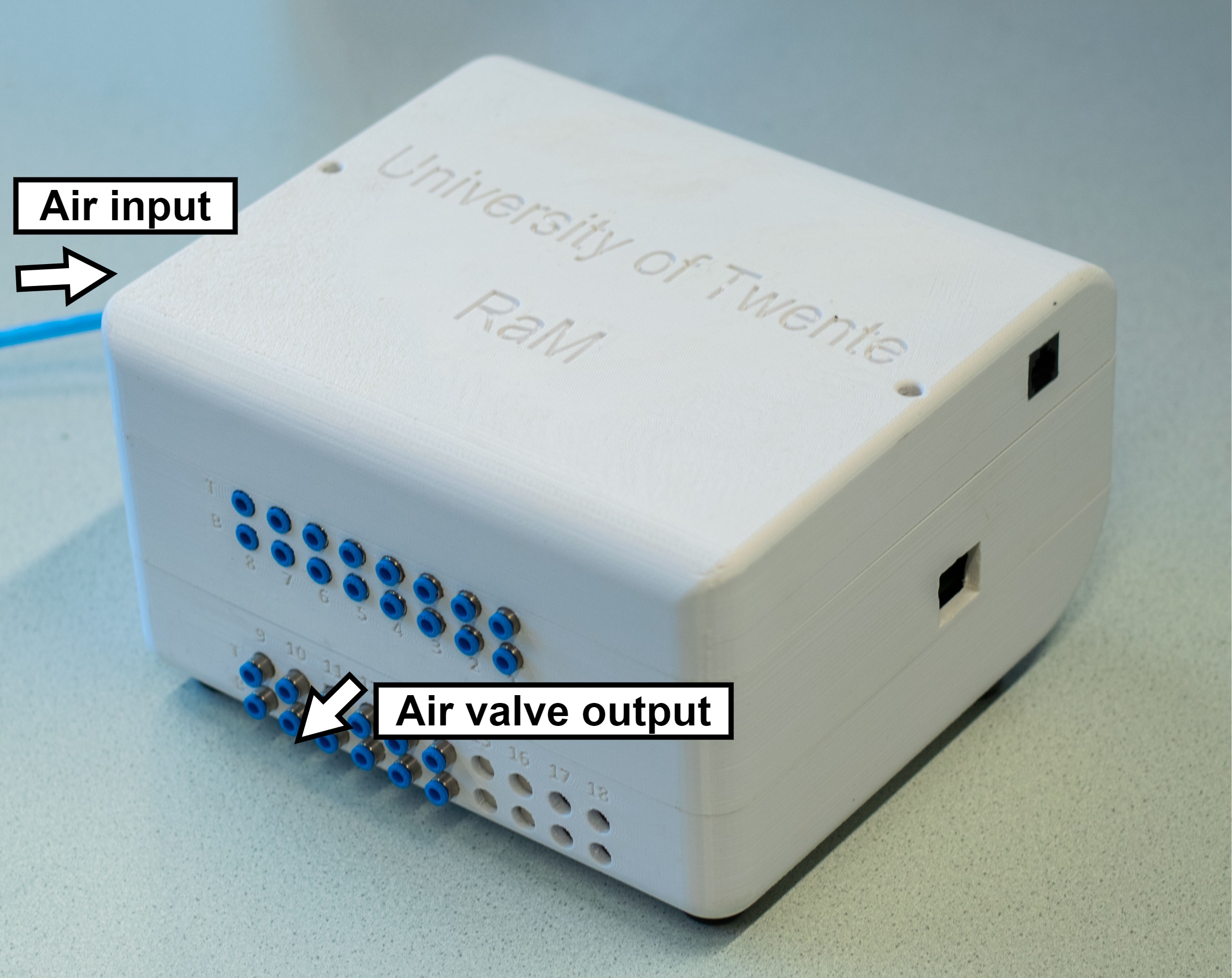
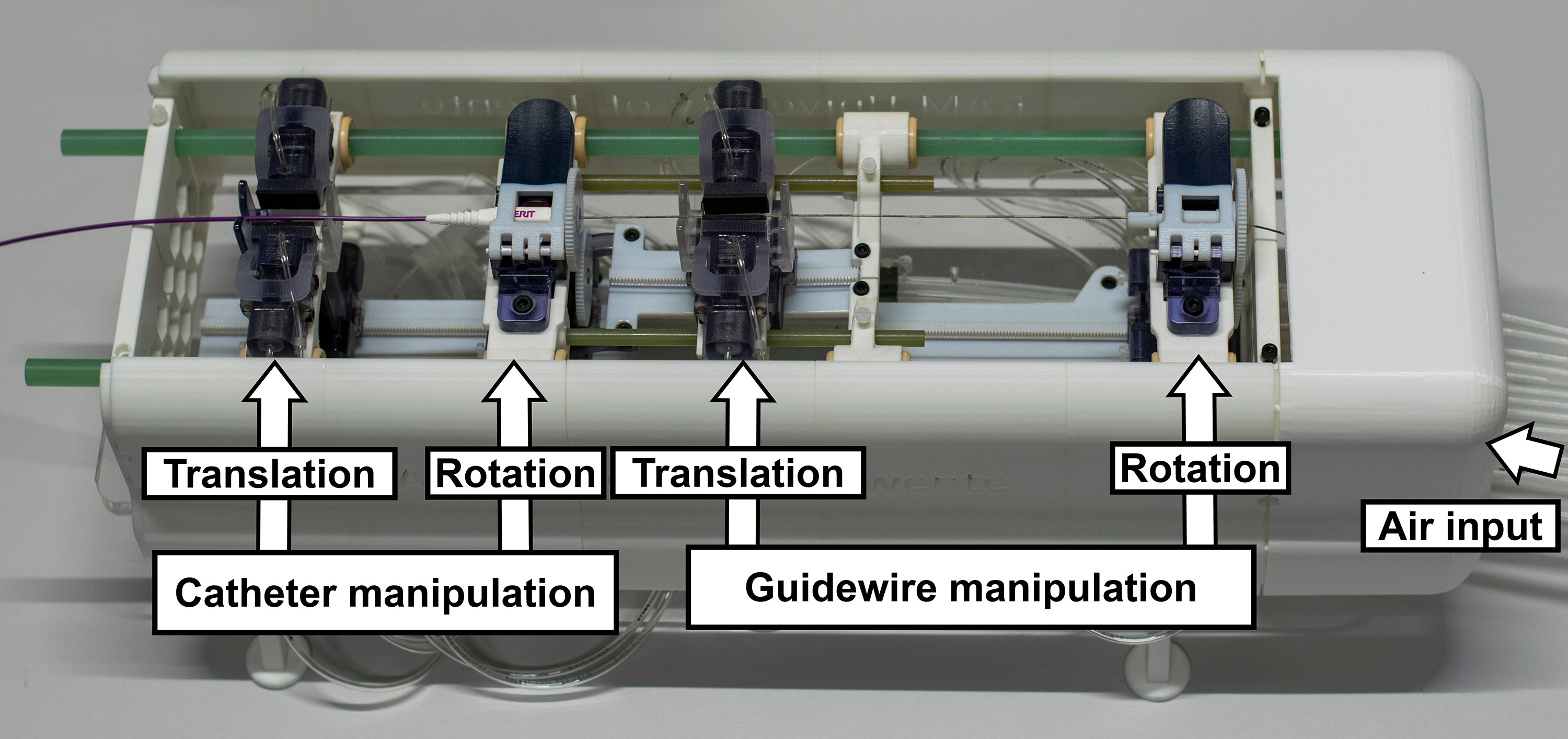
CathBot is an MR-safe robotic platform, which uses pneumatic stepper motors to rotate and translate endovascular guidewire and catheter. The MR-safe robot is controlled by an HMI called Main Controller (left). The Main Controller sends commands to a pneumatic controller (middle), which creates pneumatic pressure patterns for the MR-safe robot (right).
MR imaging
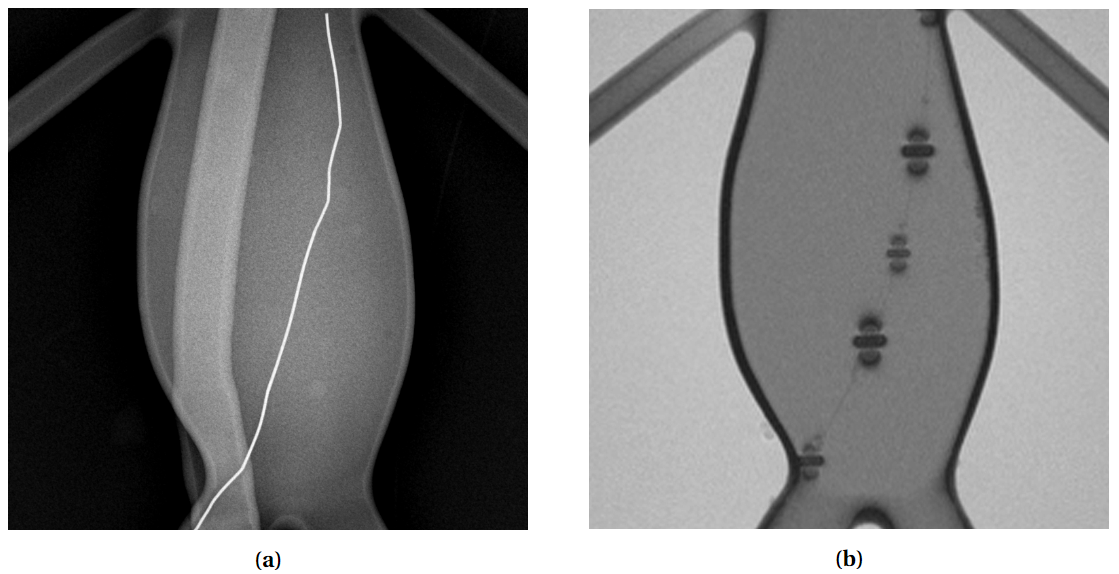
The endovascular device visibility issue is demonstrated in the image below. Additionally to the image, MRI is not a "projection" based imaging (such as X-ray), but rather can only image a thin slice of an object. Anything outside of the slice is not visible.
Project outline
The project is split into 4 phases:
- Optimizing MR sequence for interactive imaging
- Simulation of magnetic susceptibility markers
- Training a CNN on the procedurally generated dataset
- Adding haptic feedback to the CathBot
Optimizing MR sequence
With MR-imaging, higher image quality or resolution will take more time to acquire, whereas low resolution images can be acquire very quickly and provide a good image update frequency. To optimize the MR sequence, a trade-off between the quality (spatial resolution) and update frequency (temporal resolution) was found.
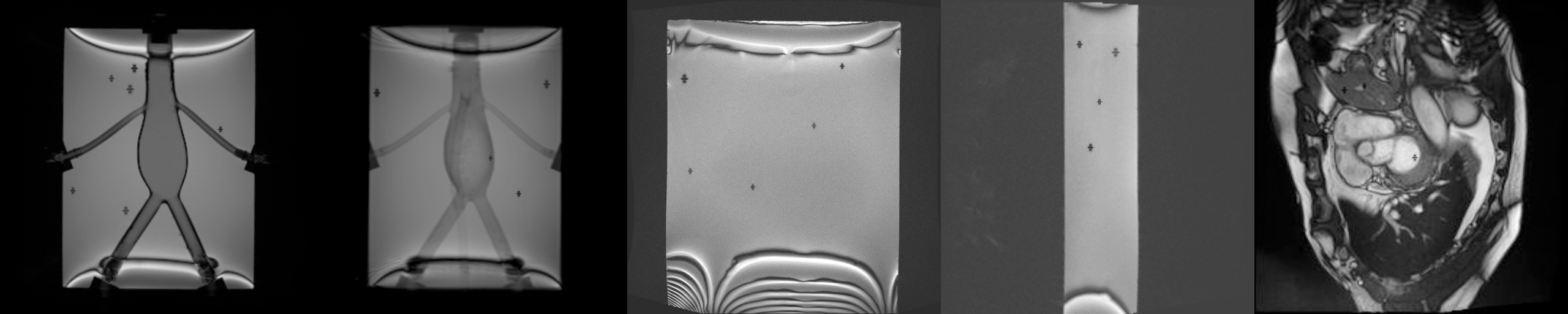
The outcome of this analysis was a bSSFP sequence with a repetition time of ~500 ms, and voxel size of 1.3 mm. Here is an example of what such sequence looks like:
Simulation of Susceptibility Markers
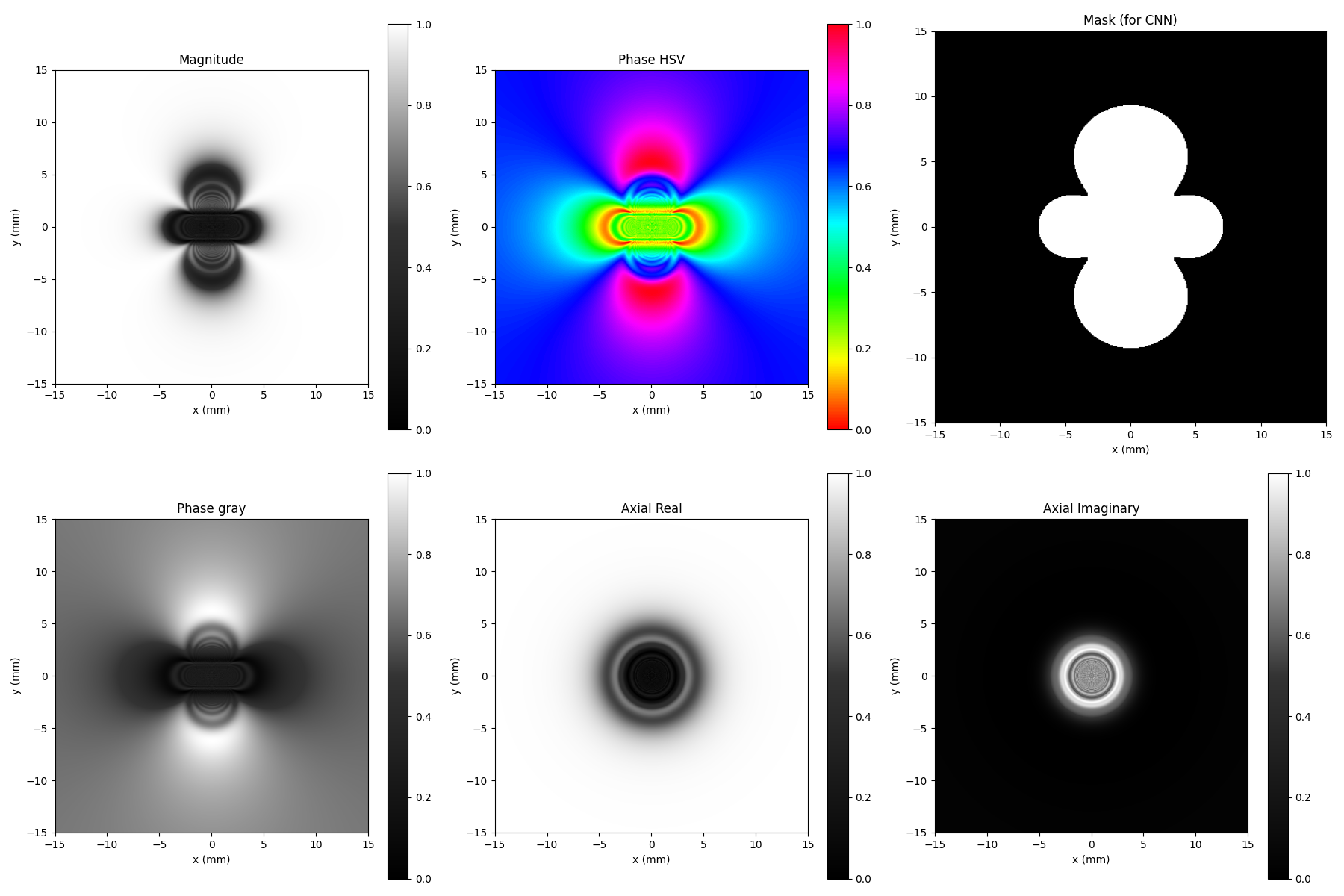
MR-safe passive guidewires have embedded markers so that the guidewires can be visible during imaging. Simulating the marker signal is necessary to procedurally generate a CNN training dataset and detect these markers during real-time imaging.
Simulated Marker
The math and implementation of these simulations are shown in the thesis.
Training CNN
The simulated marker was augmented by contrast, shape, and size and placed on various MR background images. A dataset of around 700 images was created.
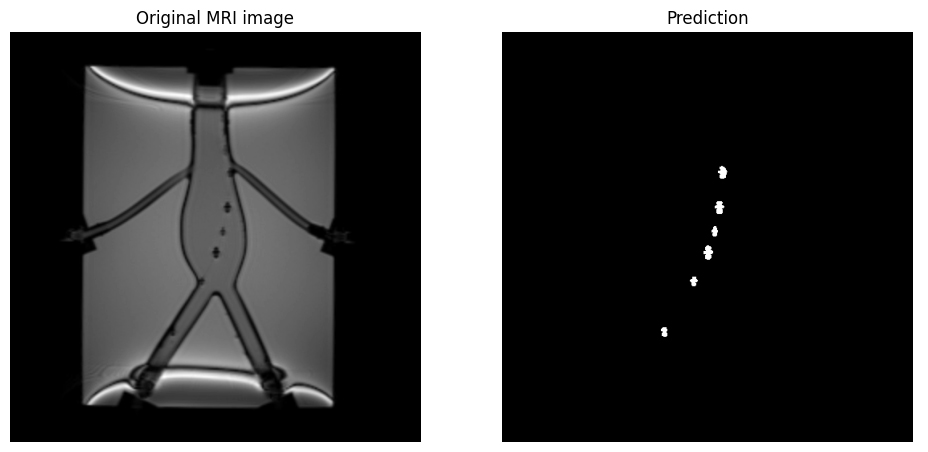
The dataset was used to train a nnU-Net model. After multiple iterations, the CNN reliably detected the markers in ~0.2 seconds. Below is an example of the detection.
The CNN performance was analyzed against manual annotation, and the results can be viewed in this Jupyter Notebook: CNN Evaluation
Here is an example of real-time CNN detection:
Safety layers
To be added.